What is myopia?
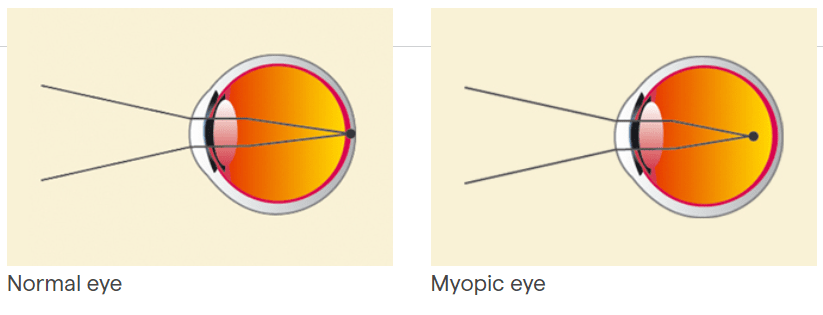
Also known as nearsightedness, it is a refractive defect or error in visual focusing, which has the following characteristics:
- Images are focused in front of the retina and not on it, making long distance vision difficult.
- It usually appears in childhood and develops approximately until the age of 20, when it tends to stabilise
- If the refractive error is greater than eight dioptres, it is referred to as high myopia, which can involve serious specific visual risks and complications.
What causes it?

- It occurs when the eyeball is elongated or the cornea is more curved than usual.
- People with a family history of myopia are more likely to suffer from it.
How can it be prevented?
It is not possible to prevent nearsightedness. Regular eye tests however, especially for children, help to detect it in its early stages.
Symptoms

A nearsighted person sees objects clearly if they are close up, but blurred if they are at a distance.
It usually appears in school-age children, so it is important to be attentive to possible symptoms.
The most common symptoms are:
- Difficulty in seeing what the teacher writes on the blackboard
- Holding books very close to the eyes to read
- Sitting close to the television
- Squinting to make distant objects appear sharper
As this refractive error develops while children are growing, it is necessary to change glasses or contact lenses frequently.
Associated treatments
It can be corrected by wearing glasses or contact lenses. People who prefer not to wear glasses or contact lenses can opt for refractive surgery.
Very rarely is surgery advisable before the age of 20, when it stabilises.
Treatment mainly consists of applying a laser to the surface or internal layers of the cornea (Lasik). Other less common techniques include the implantation of rings.
In cases of high myopia or when Lasik is contraindicated, none of these corneal procedures is recommended. The best option is the implantation of phakic intraocular lenses (between the cornea and the crystalline lens).
About 80% of the success of surgery depends on proper diagnosis and selection of the most suitable technique.
Specialists who treat this pathology
FAQs
Angiography is a technique used to delineate retinal or choroidal cases. Different contrasts are used, usually sodium fluorescein or indocyanine green. The scan is also useful for the diagnosis of other retinal diseases, such as pigment epithelium. In general, angiography is used to study many retinal diseases and their diagnosis.
Indocyanine green angiography is a technique used in some cases of AMD and serves to define the neovessels and, occasionally, to diagnose other diseases. Fluorescein angiography is the standard technique for studying blood vessel diseases and the retina in general.
It is a diagnostic technique to determine pathological and abnormal structures in the blood vessels and the different layers of the retina. It can be used in cases of macular degeneration, diabetic retinopathy, vasculopathy and many other macular disorders.
It is not counterproductive for any eye treatment.
For the first two weeks, in particular, the patient should avoid rubbing the eyes, going swimming in a public pool and using eyelid make-up.
The patient can generally have acceptable or near-maximum vision within a few hours. Occasionally, however, it can take up to a week for vision to improve.
Yes, as can all post-operative patients, irrespective of the pathology, provided that their physical condition permits and several days have passed since the operation.
Nowadays, there are several techniques. The most popular for small refractive errors, such as myopia, hyperopia and astigmatism, is LASIK. In special cases there are other options available: phakic lenses, crystalline extraction, intracorneal lenses or intrastromal rings.
IMO Institute of Ocular Microsurgery
Josep María Lladó, 3
08035 Barcelona
Phone: (+34) 934 000 700
E-mail: international@imo.es
See map on Google Maps
By car
GPS navigator coordinates:
41º 24’ 38” N – 02º 07’ 29” E
Exit 7 of the Ronda de Dalt (mountain side). The clinic has a car park with more than 200 parking spaces.
By bus
Autobus H2: Rotonda de Bellesguard, parada 1540
Autobus 196: Josep Maria Lladó-Bellesguard, parada 3191
Autobuses H2, 123, 196: Ronda de Dalt – Bellesguard, parada 0071
How to arrive at IMO from:
IMO Madrid
C/ Valle de Pinares Llanos, 3
28035 Madrid
Phone: (+34) 910 783 783
See map in Google Maps
Public transport
Metro Lacoma (líne 7)
Autobuses:
- Lines 49 & 64, stop “Senda del Infante”
- Line N21, stop “Metro Lacoma”
Timetables
Patient care:
Monday to Friday, 8 a.m. to 9 p.m.
IMO Andorra
Av. de les Nacions Unides, 17
AD700 Escaldes-Engordany, Andorra
Phone: (+376) 688 55 44
See map in Google Maps
IMO Manresa
C/ Carrasco i Formiguera, 33 (Baixos)
08242 – Manresa
Tel: (+34) 938 749 160
See map in Google Maps
Public transport
FGC. Line R5 & R50 direction Manresa. Station/Stop: Baixador de Manresa
Timetables
Monday to Friday, 09:00 A.M – 07:00 PM