What are ocular tumours?
Ocular tumours can appear on the eyelids, in the eye (conjunctiva, choroid or retina) and in the orbit (the cavity that houses the eyeball).
Given their delicate location, early diagnosis and treatment is necessary. Time is of the essence to save vision, the eye and even the life of the patient in the most serious cases.
There are several types of benign and malignant tumours that affect the eye and its different structures. The main intraocular tumours include:
- Melanoma: This can affect various tissues, although melanomas located in the choroid (choroidal melanomas) are the most common primary malignant intraocular tumour in adults. Its number of cases increases yet further if secondary tumours to other cancer processes are considered, which end up causing metastasis in the eye, such as breast or lung cancer.
- Retinoblastoma: Most common malignant eye tumour in children. It is very aggressive and, therefore, early diagnosis and treatment are essential.
- Choroidal Hemangioma: Benign tumour (no risk of metastasis) that, however, develops very quickly and aggressively, involving a risk to the eyesight because its growth threatens the optic nerve (transmitter of images from the retina to the brain) and the macula (central area of the retina that provides high-acuity vision).
What causes them?
Some tumours are congenital, such as 50% of all retinoblastomas that are passed on from one generation to another and affect 1 in every 15,000 newborns.
Others, such as intraocular melanomas, have no specific risk factors. Some can be associated with other syndromes, be secondary to conditions affecting adjacent areas or be due to a process of metastasis.
How can they be prevented?
Intraocular tumours cannot be prevented, but they can be diagnosed in their early stages. A routine annual examination of the back of the eye is therefore recommended after the age of 50, which is when this type of problems most commonly start to appear.
Furthermore, given that malignant lesions can come back over time, regularly follow-ups are important once they have been treated.
Symptoms
Given that they are internal, they are often initially unnoticed and are asymptomatic. Some warning signs that can be associated to an intraocular tumour include:
- Reduced eyesight
- Detached retina o intraocular haemorrhage
Therefore, intraocular tumours are often diagnosed during a routine ophthalmological examination.
Associated treatments
Treatment of eye tumours depends on their type, location and size. Malignant tumours generally require removal through micro-incision surgery, which may be backed up with chemotherapy or local radiotherapy in coordination with an oncologist and has a great success rate.
For choroidal melanomas, the therapy of choice is normally brachytherapy, which consists of a radioactive ruthenium or iodine plate being located in the tumoural region for a few days. Given that it is local, it avoid external radiation and reduces any side effects, making it a minimally invasive option.
Furthermore, choroidal hemangiomas are often treated using photodynamic therapy and retinoblastomas with a combination of laser chemotherapy and cryotherapy.
Specialists who treat this pathology
FAQs
Eye tumours can occur on any tissue, but the most common in adults is choroidal melanoma, a malignant tumour that can be treated with radiotherapy and other treatments with notable success. Malignant tumours can also appear on the conjunctiva, the lacrimal gland and the orbit. Benign tumours can also appear, but they can be easily dried out. In children a retinal tumour known as retinoblastoma can appear, which looks like a white pupil and must be treated as soon as possible, as it can be life-threatening if appropriate treatment is not performed.
If a patient who has been operated on for cataracts or other intraocular processes suffers a severe loss of vision with noticeable eye redness and pain, he or she must go and see an ophthalmologist urgently and without delay, as the emergency could threaten the vision of the eye.
IMO Institute of Ocular Microsurgery
Josep María Lladó, 3
08035 Barcelona
Phone: (+34) 934 000 700
E-mail: international@imo.es
See map on Google Maps
By car
GPS navigator coordinates:
41º 24’ 38” N – 02º 07’ 29” E
Exit 7 of the Ronda de Dalt (mountain side). The clinic has a car park with more than 200 parking spaces.
By bus
Autobus H2: Rotonda de Bellesguard, parada 1540
Autobus 196: Josep Maria Lladó-Bellesguard, parada 3191
Autobuses H2, 123, 196: Ronda de Dalt – Bellesguard, parada 0071
How to arrive at IMO from:
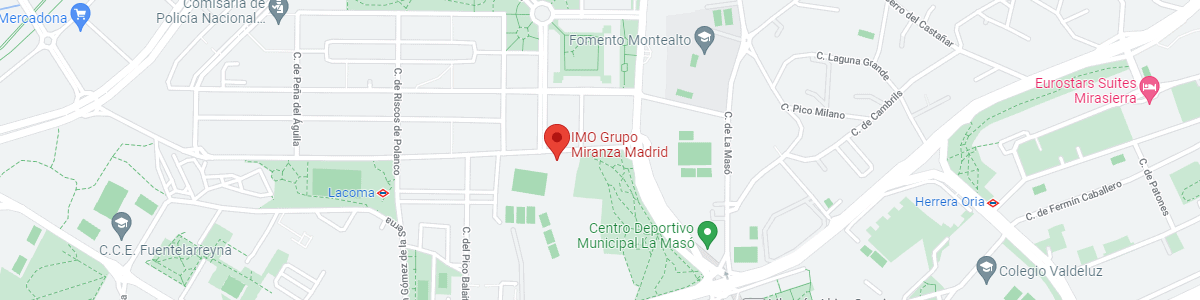
IMO Madrid
C/ Valle de Pinares Llanos, 3
28035 Madrid
Phone: (+34) 910 783 783
See map in Google Maps
Public transport
Metro Lacoma (líne 7)
Autobuses:
- Lines 49 & 64, stop “Senda del Infante”
- Line N21, stop “Metro Lacoma”
Timetables
Patient care:
Monday to Friday, 8 a.m. to 9 p.m.
IMO Andorra
Av. de les Nacions Unides, 17
AD700 Escaldes-Engordany, Andorra
Phone: (+376) 688 55 44
See map in Google Maps
IMO Manresa
C/ Carrasco i Formiguera, 33 (Baixos)
08242 – Manresa
Tel: (+34) 938 749 160
See map in Google Maps
Public transport
FGC. Line R5 & R50 direction Manresa. Station/Stop: Baixador de Manresa
Timetables
Monday to Friday, 09:00 A.M – 07:00 PM