What does it involve?
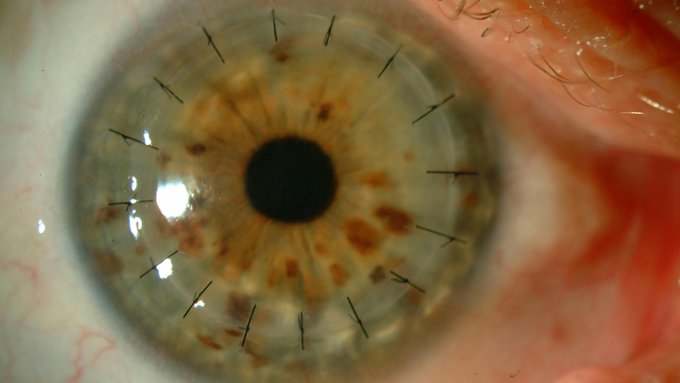
Corneal transplantation (keratoplasty) can be penetrating, when it involves replacing the entire cornea, or lamellar or selective, when only the affected layers are replaced.
Therefore, depending on the location of the damage, different lamellar transplantation types are possible:
- Endothelial corneal transplantation (DMEK): when the lesion is produced on the endothelium or innermost layer.
- Anterior corneal transplantation: when the lesion is produced in the stroma, which represents 95% of the total thickness of the cornea.
Where the epithelium, the outermost layer, is affected, a corneal stem cell transplantation is required.
When is it carried out?
Keratoplasty is performed to maintain the transparency and regularity of the cornea and is especially recommended for patients who, due to diseases such as keratoconus or due to an accident, have damaged the entire thickness of the cornea or any of its layers. In this latter case, the IMO specialists generally recommend lamellar techniques, which are less invasive than penetrating keratoplasty.
70% of all corneal transplants performed at the Institute are selective, as they are less aggressive surgeries that cut down on recover time, improve the prognosis and reduce any short and long-term complications and the risk of rejection.
Prior examination
A full ophthalmological examination and pre-operative tests must be performed.
During surgery
The surgery takes 30 to 40 minutes and is performed under local anaesthesia and sedation.
After surgery
Strenuous activity should be avoided for three weeks after surgery.
Risks
Those associated with any surgery. Despite being much lower than in the transplantation of any other tissue and having been reduced greatly thanks to selective techniques, the risk of rejection exists throughout the patient’s entire lifetime.
Associated pathologies
Experts performing this treatment
FAQs
Most patients who suffer rejection of a corneal transplantation experience reduced vision. Other symptoms include the appearance of foreign bodies and being dazzled or bothered by light.
The patient should avoid strenuous activities and, in particular, avoid direct trauma to the eye.
IMO Institute of Ocular Microsurgery
Josep María Lladó, 3
08035 Barcelona
Phone: (+34) 934 000 700
E-mail: international@imo.es
See map on Google Maps
By car
GPS navigator coordinates:
41º 24’ 38” N – 02º 07’ 29” E
Exit 7 of the Ronda de Dalt (mountain side). The clinic has a car park with more than 200 parking spaces.
By bus
Autobus H2: Rotonda de Bellesguard, parada 1540
Autobus 196: Josep Maria Lladó-Bellesguard, parada 3191
Autobuses H2, 123, 196: Ronda de Dalt – Bellesguard, parada 0071
How to arrive at IMO from:
IMO Madrid
C/ Valle de Pinares Llanos, 3
28035 Madrid
Phone: (+34) 910 783 783
See map in Google Maps
Public transport
Metro Lacoma (líne 7)
Autobuses:
- Lines 49 & 64, stop “Senda del Infante”
- Line N21, stop “Metro Lacoma”
Timetables
Patient care:
Monday to Friday, 8 a.m. to 9 p.m.
IMO Andorra
Av. de les Nacions Unides, 17
AD700 Escaldes-Engordany, Andorra
Phone: (+376) 688 55 44
See map in Google Maps
IMO Manresa
C/ Carrasco i Formiguera, 33 (Baixos)
08242 – Manresa
Tel: (+34) 938 749 160
See map in Google Maps
Public transport
FGC. Line R5 & R50 direction Manresa. Station/Stop: Baixador de Manresa
Timetables
Monday to Friday, 09:00 A.M – 07:00 PM