What is laser refractive surgery?

And in which cases is laser refractive surgery performed?
Laser-based refractive surgery techniques (such as PRK, LASIK, LASEK or EPILASIK) offer the possibility of altering the thickness and/or curvature of the cornea (and, therefore, its dioptric value) to correct refractive defects:
- myopia
- hyperopia
- astigmatism.
One of the most innovative techniques is Relex SMILE (Small Incision Lenticule Extraction) that uses the femtosecond laser and allows the surgeon to modify the cornea’s optical power through a 2mm microincision.
Laser refractive surgery can also be used to correct presbyopia or old eyes to compensate for the crystalline lens’s loss of accommodation or ability to focus close up, which appears after the age of 40-45.
When is it carried out?
In people with refractive defects who want to reduce their dependence on glasses or contact lenses. This is one of the many different surgical options that exist at present for this purpose and, therefore, the ophthalmologist must determine whether the patient is a suitable candidate for refractive surgery and, if so, select the best technique in relation to characteristics such as
- the patient’s eye
- his or her age
- personal preferences
- profession.
Prior examination
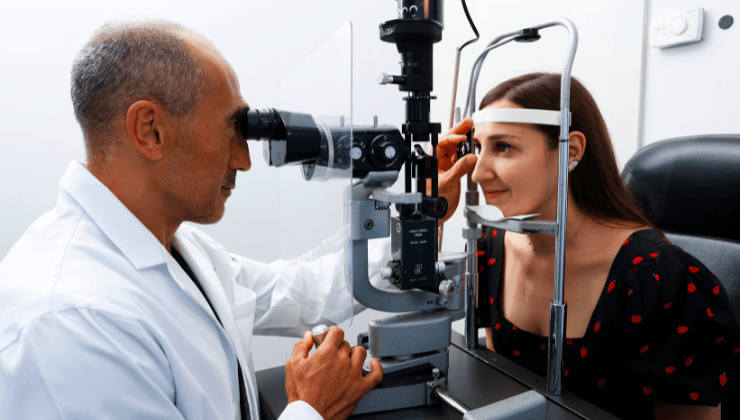
A correct indication of refractive surgery, as well as good patient-ophthalmologist communication, requires a complete ophthalmological examination and a series of pre-operative tests.
Firstly must be measured:
- visual acuity.
- refraction (degree of myopia, hyperopia, astigmatism or presbyopia) .
- intraocular pressure.
Then, a topography (measurement of the curvature and thickness of the cornea) must be performed for precise application of the laser, and a study of the corneal hysteresis, i.e. the degree of resistance and elasticity of this tissue, using a device called an ORA (Ocular Response Analyzer).
Before surgery
On the day of the surgery, the patient is called in to repeat the diagnostic tests and confirm that there have been no changes since the pre-operative visit and that the eye can be operated on.
It is important for patients to be accompanied by another person and to avoid a large breakfast or lunch and energy drinks, as they will be given a painkiller and anaesthetic drops before surgery.
During surgery
During surgery, the cooperation of the patient is required to keep looking at the microscope light. The surgery takes around five minutes and, in general, it is performed under topical anaesthesia, i.e. anaesthetic drops, meaning that there is no need to cover the eye after surgery, and the patient can see with the eye when leaving the theatre.
However, patients should spend the remainder of the day resting their eyes and keep their eyes closed for as long as possible in a dark room, applying the topical medication recommended by the ophthalmologist.
Risks
The risks of laser refractive surgery are those of any other type of surgery. Insofar as possible side effects (dry eye, halos, flashes, etc.), these are mostly temporary. The most common is dry eye, which generally disappears after a few months and for which the use of lubricating drops is recommended.
Apart from these effects, it must be remembered that laser refractive surgery produces alterations to the curvature and thickness of the cornea, which must be taken into account with regards to future diagnostic tests and pre-surgical medication.
It must also be noted that the benefits of the surgery do not last a lifetime, due to the changes that the eyes experience over the years.
Associated pathologies
Experts performing this treatment
FAQs
Nowadays, there are several techniques. The most popular for small refractive errors, such as myopia, hyperopia and astigmatism, is LASIK. In special cases there are other options available: phakic lenses, crystalline extraction, intracorneal lenses or intrastromal rings.
IMO Institute of Ocular Microsurgery
Josep María Lladó, 3
08035 Barcelona
Phone: (+34) 934 000 700
E-mail: international@imo.es
See map on Google Maps
By car
GPS navigator coordinates:
41º 24’ 38” N – 02º 07’ 29” E
Exit 7 of the Ronda de Dalt (mountain side). The clinic has a car park with more than 200 parking spaces.
By bus
Autobus H2: Rotonda de Bellesguard, parada 1540
Autobus 196: Josep Maria Lladó-Bellesguard, parada 3191
Autobuses H2, 123, 196: Ronda de Dalt – Bellesguard, parada 0071
How to arrive at IMO from:
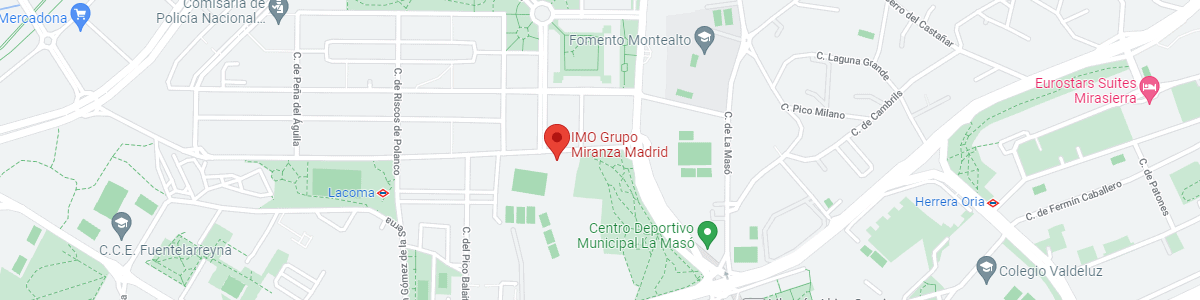
IMO Madrid
C/ Valle de Pinares Llanos, 3
28035 Madrid
Phone: (+34) 910 783 783
See map in Google Maps
Public transport
Metro Lacoma (líne 7)
Autobuses:
- Lines 49 & 64, stop “Senda del Infante”
- Line N21, stop “Metro Lacoma”
Timetables
Patient care:
Monday to Friday, 8 a.m. to 9 p.m.
IMO Andorra
Av. de les Nacions Unides, 17
AD700 Escaldes-Engordany, Andorra
Phone: (+376) 688 55 44
See map in Google Maps
IMO Manresa
C/ Carrasco i Formiguera, 33 (Baixos)
08242 – Manresa
Tel: (+34) 938 749 160
See map in Google Maps
Public transport
FGC. Line R5 & R50 direction Manresa. Station/Stop: Baixador de Manresa
Timetables
Monday to Friday, 09:00 A.M – 07:00 PM