What is uveitis?
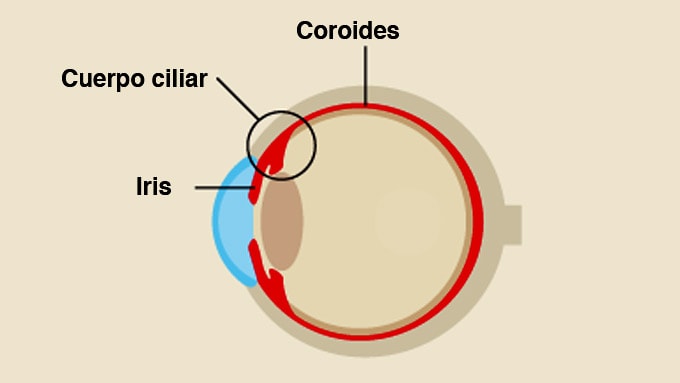
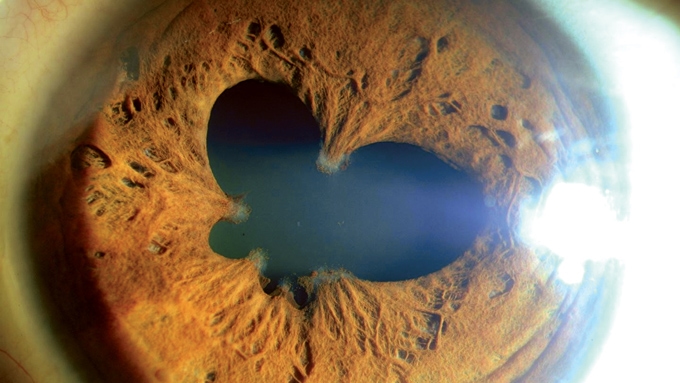
Uveitis is an inflammation of the uvea, the membrane that envelops the interior of the eyeball.
The uvea is highly sensitive to infectious and inflammatory processes as its tissue contains the greatest number of blood vessels in the human body.
Uveitis is one of the leading causes of blindness in the world. Infection of the uvea causes severe vision loss due to its contact with delicate eye structures such as the retina.
The uvea is located inside the eyeball and consists of two parts: the anterior uvea (iris and ciliary body), in contact with the crystalline lens and the structures of the anterior chamber, and the posterior uvea (choroid), in direct contact with the retina.
What causes it?
Various factors can cause uveitis:
- Infectious diseases such as toxoplasmosis (a disorder caused by a parasite that produces calcifications in the organism and scarring of the retina) can lead to the most common cause of uveitis: infectious chorioretinitis. This process causes a gradual destruction of the retina and, if it affects the macula (the central part of the retina), can cause significant and irreversible loss of vision
- Bone and rheumatic diseases that are inflammatory and non-degenerative in origin, mainly affecting young people
- Autoimmune diseases caused by viruses, bacteria or environmental factors such as sarcoidosis or Behçet’s disease, a disorder of unknown origin that causes sores and skin lesions
- Trauma or a specific genetic code associated with the disease
Uveitis is less common in the first 10 years of life and its frequency decreases from the age of 60. Most sufferers are aged between 20 and 50.
How can it be prevented?
Uveitis is one of the eye diseases that are most commonly related to other diseases of the human body.
The study and treatment of diseases that cause uveitis is usually carried out in conjunction with an internal medicine specialist. In some cases, the treatment of these diseases or infections can help to prevent it.
Símptomes
The symptoms of uveitis vary depending on the area of the uvea that is affected.
- If the anterior part is affected, symptoms include increased sensitivity to light (photophobia), redness in the eye, blurred vision or eye pain
- If the posterior part is affected, symptoms include vision loss, but probably no pain
Uveitis cannot be diagnosed until external signs appear. When the first symptoms appear, it is important to see the ophthalmologist immediately.
It is common for uveitis to be associated with bone or rheumatic diseases that are inflammatory in origin, mainly affecting young people.
Associated treatments
Various treatment options are available, depending on the type and location of the uveitis:
In most cases, anterior uveitis is treated with anti-inflammatory eye drops
Non-infectious posterior uveitis is treated with cortisone administered orally or through injections around the eye
Chronic forms of uveitis may require the use of immunomodulatory drugs
Surgery is not a conventional treatment for uveitis, but it can be effective to correct associated complications such as cataracts or glaucoma (affecting the anterior segment), retinal detachment, vitreous opacity or macular edema (affecting the back of the eye)
Specialists who treat this pathology
FAQs
Angiography is a technique used to delineate retinal or choroidal cases. Different contrasts are used, usually sodium fluorescein or indocyanine green. The scan is also useful for the diagnosis of other retinal diseases, such as pigment epithelium. In general, angiography is used to study many retinal diseases and their diagnosis.
Indocyanine green angiography is a technique used in some cases of AMD and serves to define the neovessels and, occasionally, to diagnose other diseases. Fluorescein angiography is the standard technique for studying blood vessel diseases and the retina in general.
It is a diagnostic technique to determine pathological and abnormal structures in the blood vessels and the different layers of the retina. It can be used in cases of macular degeneration, diabetic retinopathy, vasculopathy and many other macular disorders.
It is not counterproductive for any eye treatment.
The head should normally be tilted forward so that the gas does not contact the front of the eye, but the surface of the back of the eye. The length of time that the head should be kept in this position depends on the quantity of gas given.
IMO Institute of Ocular Microsurgery
Josep María Lladó, 3
08035 Barcelona
Phone: (+34) 934 000 700
E-mail: international@imo.es
See map on Google Maps
By car
GPS navigator coordinates:
41º 24’ 38” N – 02º 07’ 29” E
Exit 7 of the Ronda de Dalt (mountain side). The clinic has a car park with more than 200 parking spaces.
By bus
Autobus H2: Rotonda de Bellesguard, parada 1540
Autobus 196: Josep Maria Lladó-Bellesguard, parada 3191
Autobuses H2, 123, 196: Ronda de Dalt – Bellesguard, parada 0071
How to arrive at IMO from:
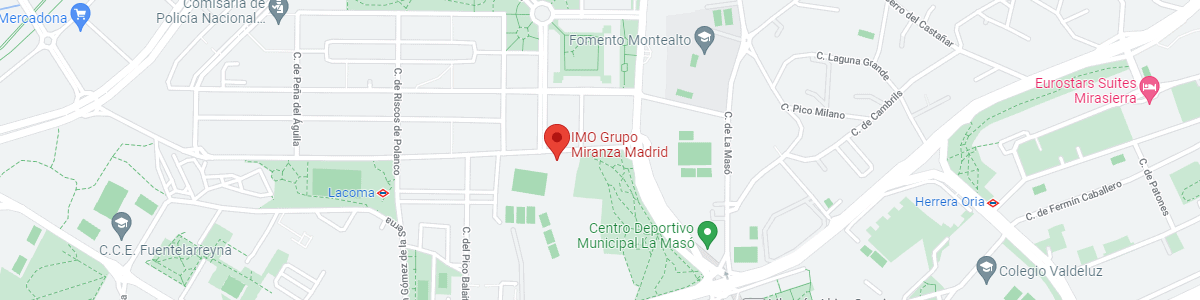
IMO Madrid
C/ Valle de Pinares Llanos, 3
28035 Madrid
Phone: (+34) 910 783 783
See map in Google Maps
Public transport
Metro Lacoma (líne 7)
Autobuses:
- Lines 49 & 64, stop “Senda del Infante”
- Line N21, stop “Metro Lacoma”
Timetables
Patient care:
Monday to Friday, 8 a.m. to 9 p.m.
IMO Andorra
Av. de les Nacions Unides, 17
AD700 Escaldes-Engordany, Andorra
Phone: (+376) 688 55 44
See map in Google Maps
IMO Manresa
C/ Carrasco i Formiguera, 33 (Baixos)
08242 – Manresa
Tel: (+34) 938 749 160
See map in Google Maps
Public transport
FGC. Line R5 & R50 direction Manresa. Station/Stop: Baixador de Manresa
Timetables
Monday to Friday, 09:00 A.M – 07:00 PM