What is glaucoma?
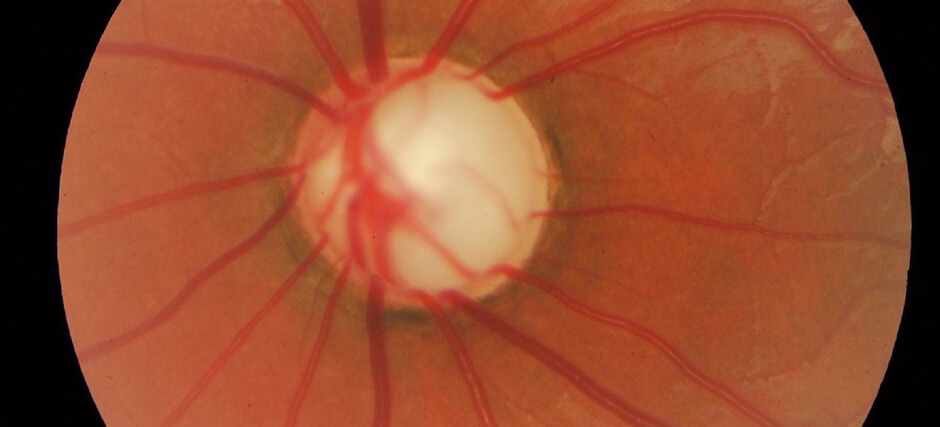
Glaucoma is one of the most common causes of blindness and comprises a group of diseases that cause progressive and irreversible damage to the optic nerve. This structure is key to vision since, through it, the images captured by the retina (converted into nerve impulses) are transmitted to the brain so that it can interpret them and generate vision.
Visual impairment
Glaucoma is a chronic disease caused by the early death of retinal ganglion cells, whose axons form the optic nerve.
As a consequence, the optic nerve loses its functionality. If the disease is not treated in time, the patient’s field of vision is reduced.
What causes glaucoma?
Most common risk factor
The main risk factor that can trigger glaucoma is ocular hipertension. This condition usually occurs because, the aqueous humor (fluid that bathes the inner eye) does not drain properly and builds up, putting excessive pressure on the optic nerve and causing a “stress” that it cannot withstand.
Other risk factors
However, there are people with elevated intraocular pressure who do not develop glaucoma and patients with normal values (less than 21 mm Hg pressure) who, on the contrary, develop the pathology.
It must be taken into account that glaucoma is not only the consequence of a “mechanical” defect in the drainage system of the aqueous humor, but it is also a multifactorial disease whose origin is still little known. Research is being carried out in this field and it is suspected that vascular problems may be associated with cases of glaucoma with normal intraocular pressure, since the blood vessels inside the eyeball are among the finest in the body and therefore particularly fragile.
Hereditary factors
On the other hand, genetic predisposition is a major factor in certain types of glaucoma, such as open-angle (familial) primary glaucoma – the most common – or congenital glaucoma – which appears in the first months of life – and juvenile glaucoma.
How can glaucoma be prevented?
After the age of 40, it is important to undergo a complete eye examination every one or two years. If eye pressure can be reduced in the early stages of glaucoma, the development of the disease can be stopped and vision can be protected.
The importance of early diagnosis
The key to avoiding irreversible damage to the optic nerve caused by glaucoma is the early diagnosis of the disease, with the aim to control it before it continues to progress. Given that in most cases it does not cause symptoms until advanced stages of the pathology, every two years check-us are recomended for people from the age of 40, as, from that age the degenerative process of the eye is activated and the incidence of glaucoma begins to increase.
Regular check-ups
Check-ups are specially recomended on people with any of the following risk factors:
- Age (over 60)
- Family history of glaucoma
- Ocular hypertension
- Myopia or high myopia
- Other eye diseases, such as corneal, retinal, uveitis, etc.
- Ocular traumas
- Narrow iridocorneal angle (formed by the cornea and sclera with the iris)
- Black or Asian race
Last generation equipment
Advances in diagnostic equipment have helped to detect glaucoma at very early stages.
A correct diagnosis is essential, including a funduscopic exploration as well as an optical nerve examination.
The following tests are usually performed:
- Posterior Optical Coherence Tomography (OCT) and HRT, to detect alterations in the posterior areas of the eye (retina and optic nerve)
- Tonometry or intraocular pressure measurement
- Pachymetry, which allows the measurement of the thickness of the cornea
- Gonioscopy, to correctly explore the iridocorneal angle
- Campimetry, to evaluate the visual field
Symptoms
A silent disease
50 % of patients with glaucoma are unaware of it, as there are usually no obvious symptoms, such as pain or sudden loss of vision. Symptoms such as reddening of the eye and severe pain, accompanied by nausea, vomiting and blurred vision, only occur in cases of an acute glaucoma attack.
Despite going unnoticed until the damage is significant the disease continues to advance, potentially affecting the patient’s daily activities and making others dangerous, such as driving.
Most frequent symptoms
Most patients with glaucoma have the following symptoms:
- loss of peripheral vision or vision of the visual field
- in some cases, there is loss of central vision, in the early stages
- falls, since glaucoma increases the risk of this type of accident by a factor of four
- acute angle-closure glaucoma attacks can produce:
- red eye
- severe pain
- blurry eyesight
- halos around the lights
- nausea or vomiting
In most cases, patients are not aware that they are suffering from glaucoma until much of the visual field has been lost.
Associated treatments
Glaucoma is a chronic pathology that currently cannot be cured. However, this is due to the fact that it is not possible to regenerate the optic nerve and recover the vision that has been lost. However, the disease is tried to be controlled by different therapeutic options, which aim to preserve the patient’s vision at the time of diagnosis.
Objective: to reduce intraocular pressure
The only effective method of stopping glaucoma is by reducing intraocular pressure. The most common treatments are as follows: ocular hypotensive drugs; laser treatment, with procedures such as endocyclophotocoagulation with diode laser; minimally invasive surgeries such as non-penetrating deep sclerectomy, trabeculectomy or drainage devices or valves, as well as MIGS (Minimally Invasive Glaucoma Surgery).
Patients with normal eye pressures
Reducing intraocular pressure has also been shown to be effective in patients suffering from glaucoma without ocular hypertension (normotensive glaucoma).
This is because when the optic nerve is damaged, even normal pressure can contribute to its further and faster deterioration, so lowering it is the only way to slow down the pathology.
Future therapies
Currently, complementary treatment approaches, such as neuroprotection, are being studied.
This treatment aims to prevent the premature death of retinal ganglion cells and the damage to the optic nerve that causes their loss. Although conclusive results in clinical practice have not yet been obtained, ongoing research has shown the following benefits of these substances: they directly protect the optic nerve and they neutralize damaging toxins, such as oxygen free radicals, responsible for cellular aging due to oxygen, more present in eyes with open-angle glaucoma than in healthy patients.
Specialists who treat this pathology
FAQs
No very complex or painful examinations are required to detect glaucoma and determine its type and stage. The most important tests when making the diagnosis include an examination of the optic nerve –either directly or using automated tests such as the OCT– and the measuring of intraocular pressure (tonometry). In addition to these, a visual field test is performed to determine the stage of the disease, visualisation of the angle formed by the cornea, iris and sclera to classify the type of glaucoma (gonioscope) and measurement of the corneal thickness, as this can have an impact on intraocular pressure (pachymetry).
Glaucoma causes a progressive decrease in the patient’s visual field, and his or her peripheral vision is gradually reduced. It is therefore difficult to notice this gradual loss until the disease is at an advanced stage and the visual field has been greatly and irreversibly reduced.
The myth of people with glaucoma seeing a black tunnel is not true, as the “appearance” of the disease varies depending on each person and the extent to which the visual field is affected. Some patients describe blurred vision, mistiness or blind spots, although they often find it difficult to explain what is wrong and may confuse glaucoma with other eye diseases such as cataracts.
It is an important factor in glaucoma, although the genetic bases of the disorder are heterogeneous: there are some cases of direct transmission from generation to generation (such as congenital glaucoma) and other cases of complex inheritance (e.g. pseudoexfoliation glaucoma) where a higher percentage of sufferers in the same family than the population average is observed. In both circumstances, genetic studies provide the opportunity to detect possible future cases of glaucoma.
While genetic research continues to progress to increase knowledge in this field, it is important for patients with a family history of glaucoma to be aware of the greater risk they are at to suffer the disease. It is therefore recommendable for people with sufferers of glaucoma in their family (parents, siblings and/or children) to take annual ophthalmological controls from the age of 40 at the very latest.
The visual field is the space covered by the vision of the eye when it is static and viewing a fixed point. Typically, the perimeter of the visual field and sensitivity within the different areas of the perimeter are assessed.
An increase in eye pressure is a result of several factors which can be summarised as mechanisms that prevent intraocular fluid (aqueous humour) from being removed properly through the normal channel. This can be mild and chronic—chronic glaucoma—or sudden, due to other processes. The ophthalmologist has to examine the patient urgently, especially in the event of acute forms.
Patients can notice small floating objects, which are capsular remains in the vitreous space, but after a few days they normally disappear. Photocoagulation with YAG laser is applied to the capsule holding the artificial intraocular lens, which over time becomes opaque, resulting in the patient losing vision. Photocoagulation with YAG laser is painless and quickly achieves visual improvement.
The width of our horizontal visual field is 200º, whereas the vertical is 130º in normal conditions.
IMO Institute of Ocular Microsurgery
Josep María Lladó, 3
08035 Barcelona
Phone: (+34) 934 000 700
E-mail: international@imo.es
See map on Google Maps
By car
GPS navigator coordinates:
41º 24’ 38” N – 02º 07’ 29” E
Exit 7 of the Ronda de Dalt (mountain side). The clinic has a car park with more than 200 parking spaces.
By bus
Autobus H2: Rotonda de Bellesguard, parada 1540
Autobus 196: Josep Maria Lladó-Bellesguard, parada 3191
Autobuses H2, 123, 196: Ronda de Dalt – Bellesguard, parada 0071
How to arrive at IMO from:
IMO Madrid
C/ Valle de Pinares Llanos, 3
28035 Madrid
Phone: (+34) 910 783 783
See map in Google Maps
Public transport
Metro Lacoma (líne 7)
Autobuses:
- Lines 49 & 64, stop “Senda del Infante”
- Line N21, stop “Metro Lacoma”
Timetables
Patient care:
Monday to Friday, 8 a.m. to 9 p.m.
IMO Andorra
Av. de les Nacions Unides, 17
AD700 Escaldes-Engordany, Andorra
Phone: (+376) 688 55 44
See map in Google Maps
IMO Manresa
C/ Carrasco i Formiguera, 33 (Baixos)
08242 – Manresa
Tel: (+34) 938 749 160
See map in Google Maps
Public transport
FGC. Line R5 & R50 direction Manresa. Station/Stop: Baixador de Manresa
Timetables
Monday to Friday, 09:00 A.M – 07:00 PM