Keys to keeping dry eye under control
12 de April de 2022
Dry eye syndrome is an extremely common disorder of the ocular surface, which affects more than a quarter of the population. Although it cannot be cured because it is a chronic problem, it can be controlled in order to reduce eye discomfort, vision problems and injuries to the cornea and conjunctiva.
To that end, it is essential for the ophthalmologist to obtain an accurate diagnosis and pursue a tailored therapeutic strategy. With regard to fulfilling treatment and ensuring that preventative measures are taken, the role of the patient is key. The IMO’s Dry Eye Area (new) seeks to accompany and provide support to patients between appointments through the offering of personalised guidance and recommendations to follow.
Here are 8 key tips from our specialists to minimise the impact of ocular dryness on visual health and quality of life:
1. Eyelid hygiene
It is important to ensure good eyelid hygiene by removing excess bacteria and oil from the eyelid edges and preventing deterioration of tear quality.
Follow these three steps to achieve good results:
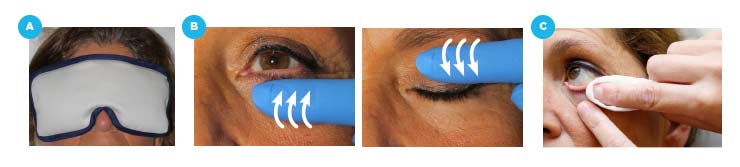
- Apply heat to the eyelids with warm swabs with the eyes closed for 5 minutes.
- Massage the eyelids, making vertical movements towards the eyelid margin (near the eyelashes). This will help release bacteria and oil.
- Clean the edge of the eyelids with soap solution applied to the root of the eyelashes or using special eyelid hygiene wipes.
In addition to being consistent in this daily care at home, carrying out regular consulting room treatments, such as eyelid microexfoliation or thermal pulsation, can help to reinforce eyelid hygiene.

2. Contact lenses
Contact lens wearers should take precautions to prevent ocular dryness. A first step is to consult with specialists on the most suitable type of contact lenses for each case, always use them correctly (do not put them in immediately after waking up, do not sleep or bathe with them in, do not overuse them, etc.) and ensure that they are properly maintained and always kept moist.

3. Environmental measures
Environmental measures also have an influence on the challenge of keeping dry eye under control. Above all, it is advisable to:
- Avoid heating and air conditioning
- Use humidifiers
- Protect the eyes with glasses that feature adequate sunscreens
- Protect the eyes in polluted or dusty environments
- Hydrate the eyes with artificial tears without preservatives

4. Habits
There are habits that are especially harmful for patients with this syndrome and should be avoided, such as rubbing the eyes, a common reaction to itching, eye fatigue or foreign body sensation, which, if done repeatedly, can weaken the cornea and increase the risk of developing keratoconus.
By contrast, it is advisable to adopt other habits that are beneficial for eye health, such as taking visual breaks every 20 minutes, when carrying out near vision activities (reading, computer work, looking at a mobile phone, etc.). In these situations, blinking decreases by up to 30%, resulting in faster tear evaporation and dry eyes.

5. Omega-3 fatty acid supplements
The consumption of food supplements rich in omega-3 fatty acids in high quantities helps to improve tear quality and has an anti-inflammatory effect, which can be highly beneficial, since most patients with dry eye have inflammation of the ocular surface.

6. Anti-inflammatories
The use of anti-inflammatories is only recommended in specific cases and they should always be prescribed by a specialist, whether they are administered sporadically or chronically (usually indicated in patients with blepharitis or patients with severe dry eye associated with Sjögren’s syndrome).
7. Antibiotics
Topical or oral antibiotics should also only be taken if prescribed by a specialist (in this case, usually indicated for blepharitis).
8. Regular eye check-ups
In addition to visits for appropriate consulting room treatments, it is advisable for patients to have regular check-ups approximately every 3-6 months for thorough monitoring of the disorder, which, thanks to the IMO’s team of specialist optometrists, is complemented by telephone consultations to discuss patient evolution, treatment guidelines, etc.

IMO Institute of Ocular Microsurgery
Josep María Lladó, 3
08035 Barcelona
Phone: (+34) 934 000 700
E-mail: international@imo.es
See map on Google Maps
By car
GPS navigator coordinates:
41º 24’ 38” N – 02º 07’ 29” E
Exit 7 of the Ronda de Dalt (mountain side). The clinic has a car park with more than 200 parking spaces.
By bus
Autobus H2: Rotonda de Bellesguard, parada 1540
Autobus 196: Josep Maria Lladó-Bellesguard, parada 3191
Autobuses H2, 123, 196: Ronda de Dalt – Bellesguard, parada 0071
How to arrive at IMO from:
IMO Madrid
C/ Valle de Pinares Llanos, 3
28035 Madrid
Phone: (+34) 910 783 783
See map in Google Maps
Public transport
Metro Lacoma (líne 7)
Autobuses:
- Lines 49 & 64, stop “Senda del Infante”
- Line N21, stop “Metro Lacoma”
Timetables
Patient care:
Monday to Friday, 8 a.m. to 9 p.m.
IMO Andorra
Av. de les Nacions Unides, 17
AD700 Escaldes-Engordany, Andorra
Phone: (+376) 688 55 44
See map in Google Maps
IMO Manresa
C/ Carrasco i Formiguera, 33 (Baixos)
08242 – Manresa
Tel: (+34) 938 749 160
See map in Google Maps
Public transport
FGC. Line R5 & R50 direction Manresa. Station/Stop: Baixador de Manresa
Timetables
Monday to Friday, 09:00 A.M – 07:00 PM