What does it involve?
This treatment involves destroying the intraocular tumours from the ocular surface without invading the eyeball. In principle, the scleral surgery technique is used primarily in melanin-type tumours, such as choroidal melanomas and, in some cases, vascular or metastatic tumours. The technique involves using, in most cases, a radioactive ruthenium-106, or sometimes an iodine-125, plaque. These plaques are placed on the surface of the eye, adjacent to the tumour.
When is it carried out?
The tumours that are treated in most cases are choroidal melanomas and metastatic and vascular tumours.
Prior examination
Prior to treating the tumour, it is very important to know the diagnosis as well as whether the tumour has spread to the rest of the body, or if the tumour is the metastasis of a primary tumour in another location. It is, therefore, essential to perform a full-body PET-CT screening test to detect for tumours that are larger than 5 mm in all organs of the body. It is also possible to carry out blood tests to assess the functioning of some organs and check for primary tumours.
Before the surgery
The most important precaution to take is to prevent tumour spread, and, to do so, it is essential to perform the technique with a microscope, as it is very delicate, and to have a good knowledge of the anatomy of the eyeball.
Surgery
The procedure is performed under local anaesthesia and involves dissecting the outer layer of the eyeball, the conjunctiva, and Tenon’s capsule to enable access to the sclera, the white wall of the eyeball. It is in the sclera that the radioactive plaque is placed after locating the tumour. The tumour is located by means of a magnifying glass for examining the fundus or transillumination, in which the pigmented nature of choroidal melanomas produce a very opaque transillumination in contrast to the white wall of the eyeball. In some cases, it is also necessary to apply other scleral techniques, such as the implantation of silicone rings, to release tension on the retina caused by tumours, laser photocoagulation or trans-scleral cryotherapy.
Risks
The main risk is tumour spread, but other risks include haemorrhaging in the vitreous cavity, retinal detachment and infections, although they are much less common.
Associated pathologies
Experts performing this treatment
FAQs
If a patient who has been operated on for cataracts or other intraocular processes suffers a severe loss of vision with noticeable eye redness and pain, he or she must go and see an ophthalmologist urgently and without delay, as the emergency could threaten the vision of the eye.
IMO Institute of Ocular Microsurgery
Josep María Lladó, 3
08035 Barcelona
Phone: (+34) 934 000 700
E-mail: international@imo.es
See map on Google Maps
By car
GPS navigator coordinates:
41º 24’ 38” N – 02º 07’ 29” E
Exit 7 of the Ronda de Dalt (mountain side). The clinic has a car park with more than 200 parking spaces.
By bus
Autobus H2: Rotonda de Bellesguard, parada 1540
Autobus 196: Josep Maria Lladó-Bellesguard, parada 3191
Autobuses H2, 123, 196: Ronda de Dalt – Bellesguard, parada 0071
How to arrive at IMO from:
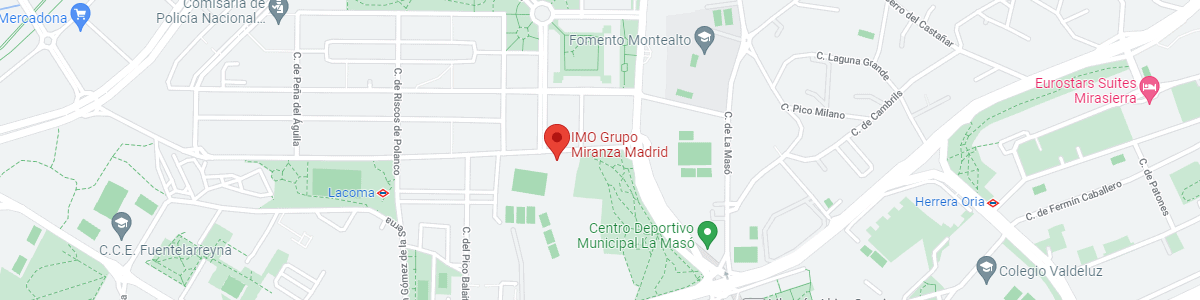
IMO Madrid
C/ Valle de Pinares Llanos, 3
28035 Madrid
Phone: (+34) 910 783 783
See map in Google Maps
Public transport
Metro Lacoma (líne 7)
Autobuses:
- Lines 49 & 64, stop “Senda del Infante”
- Line N21, stop “Metro Lacoma”
Timetables
Patient care:
Monday to Friday, 8 a.m. to 9 p.m.
IMO Andorra
Av. de les Nacions Unides, 17
AD700 Escaldes-Engordany, Andorra
Phone: (+376) 688 55 44
See map in Google Maps
IMO Manresa
C/ Carrasco i Formiguera, 33 (Baixos)
08242 – Manresa
Tel: (+34) 938 749 160
See map in Google Maps
Public transport
FGC. Line R5 & R50 direction Manresa. Station/Stop: Baixador de Manresa
Timetables
Monday to Friday, 09:00 A.M – 07:00 PM